World Stroke Day will be observed one week from today, on October 29th, as a way to raise awareness of this dangerous medical emergency.
A stroke occurs when blood flow to a portion of the brain is cut off. Lack of blood flow means that brain cells are starved of oxygen, causing them to die. Strokes kill approximately 140,000 people in the United States each year (about 1 of every 20 deaths). Someone in the U.S. suffers a stroke approximately every 40 seconds, with a fatal stroke occurring every 4 minutes.
There are three main types of stroke. The most common, ischemic stroke, occurs when a blockage of some sort (often a blood clot) prevents oxygen from reaching the brain. Hemorrhagic strokes occur when blood vessels rupture or leak, and the resulting pressure damages the brain cells surrounding the bleeding. The final type, a transient ischemic attack (TIA) — often referred to as a “mini” stroke because it’s a short-term interruption of blood flow — is usually caused by a blood clot or other blockage, and is a serious warning sign of a future stroke. According to the CDC, more than a third of people who don’t seek treatment after a TIA episode will suffer a major stroke within a year.
We’ve established that strokes are quite common, but some people are obviously at higher risk than others. What factors make an individual more likely to suffer from a stroke?
The most important risk factors are:
- High blood pressure is the single most important risk factor for stroke. If your blood pressure consistently measures above 140/90, you should talk with your doctor to see if lifestyle changes or medication could lower your blood pressure and, as a result, your risk of stroke.
- Heart disease is a risk factor when it causes blood clots, potentially leading to a stroke.
- Diabetes.
- Age: the risk of stroke increases as you get older. Almost 75% of all strokes occur in people over 65, with the risk almost doubling each decade after age 55.
- Gender. When a young person has a stroke, the victim is more likely to be male. However, around 425,000 American women have a stroke each year — about 55,000 more than men. Women are also more likely to to die as a result of stroke.
- Race / ethnicity. Strokes occur more frequently in adults of African American, Native Alaskan, and Native American descent than in Caucasian, Hispanic, or Asian American populations.
- Personal or family medical history. A family history of stroke increases an individual’s risk. In addition, a stroke survivor has a greater-than-average chance of suffering another one, and anyone who has a brain aneurysm (a bulge in an artery that can burst under pressure) or arteriovenous malformation (tangled masses of blood vessels in the brain that can rupture) is also at greater risk for stroke.
- Smoking (including secondhand exposure) causes cardiovascular damage and can reduce the amount of oxygen regularly available to cells. Smoking-related damage to blood vessels can raise blood pressure and increase the risk of stroke.
- Medications. Using non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and naproxen — but not aspirin, which is also an NSAID — has been linked to stroke, especially in patients with a prior heart attack or cardiac bypass. There’s evidence that the danger gets higher with long-term NSAID use. Taking birth control pills puts women at slightly greater risk of stroke, too.
Other risk factors for stroke include: excess body weight or obesity; suffering from stress and depression; high cholesterol / triglyceride levels; leading a sedentary lifestyle with very little physical exercise; poor dietary choices; and consuming alcohol and illegal drugs.
While it’s good to understand how risk factors can affect the likelihood of stroke, it is arguably more important to understand the signs that can indicate someone is suffering a stroke. The most common ones are:
- Sudden, painful headache with no known cause.
- Dizziness, lack of balance, or trouble walking or speaking that occurs suddenly.
- Difficulty with eyesight, affecting one or both eyes.
- Confusion, feeling disoriented.
- Struggling to speak or understand what is being said.
- Sudden weakness or feeling of numbness, especially if it only affects one side of the body.
A person exhibiting signs of a stroke is a medical emergency, and it is crucial to get treatment as soon as possible. Delaying medical care increases the risk of permanent brain damage or death. If you are with someone who begins to show any of the above signs, remembering the acronym “F.A.S.T.” can help you quickly evaluate whether they may need medical attention. The letters in “F.A.S.T.” stand for:
- F — for FACE. If someone is showing signs of suffering a stroke, ask the person to smile. If one side of their face droops or doesn’t look like the other half, or if they tell you their face feels numb on one side, this is a classic warning sign.
- A — for ARMS. Ask the possible victim to raise both arms. If they cannot lift one arm because it feels weak or numb, or if one of their arms begins to move downward after they lift it, get help!
- S — for SPEECH. Ask the person to repeat a simple sentence like, “My name is Mary Baker.” If they cannot repeat the sentence, or if their words are slurred or difficult to understand, they need immediate medical attention.
- T — for TIME … as in, time is absolutely critical if the person shows ANY of the symptoms in the first three steps. Even if the symptoms seem to improve (or go away entirely), please call 911 and get them to the hospital immediately for evaluation.
If you believe someone is showing symptoms of a stroke, how do you increase the chances that they will survive? The absolute best way is to call 911 and get emergency transportation to a hospital. While it may be tempting to think that you can get the victim there before an ambulance will arrive, it’s important to remember that paramedics and EMTs are trained to evaluate and treat medical emergencies, and to gather information that allows patients to be treated more effectively when they reach the Emergency Room. Research proves that, as a general rule, stroke patients receive critical treatment (including potentially life-saving medication) and reach the hospital faster when they are transported in an ambulance.
Although it’s easy to think that we’ll scare our kids by talking about what to do in case of a medical emergency, certainly tweens and teens are old enough to learn the signs of stroke and how to determine whether they should call 911. I’d encourage you to download the printable “F.A.S.T.” guide that we’ve created, talk to your kids about the information found on it, and display it on your refrigerator or somewhere else that’s easily accessible. When you consider that a neighbor or relative — or even you — could suffer a stroke at some point and need life-saving help, equipping your kids to deal with this type of emergency is one of the kindest and most responsible things you can do for them. 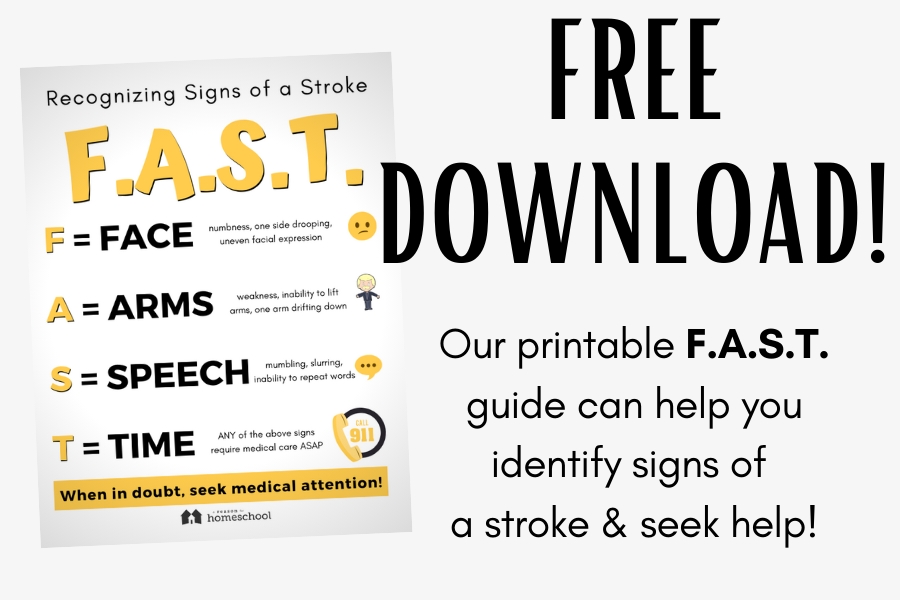
Download your free copy today:
Printable F.A.S.T. Guide
You may be asked to enter your email address if we don’t recognize you as a current subscriber.
Once you have, you can simply return to this page to download the file!
We invite you to visit their website to learn more about their excellent homeschooling resources.

